A single climate change module integrated into an advanced pharmacology course for advanced practice registered nursing students enhanced their knowledge and attitudes toward sustainability and climate change. This small-scale intervention may serve as an example for other healthcare professionals (HCPs) to successfully integrate climate change education into their curricula.
Introduction: Climate change plays a critical role in global health, emphasizing the urgent need to integrate climate change education into healthcare professional curricula. This small pilot study evaluated the integration of climate change education into an Advanced Pharmacology course for advanced practice registered nurse students.
Methods: Pre- and post-lecture surveys were used to assess changes in student knowledge and attitude regarding climate change and sustainability in healthcare.
Results: Significant improvements were noted in students’ knowledge about drug classes affecting sweating/hyperhidrosis (p < 0.001) and in attitudes toward the importance of climate change in nursing education (p < 0.05).
Conclusion: These findings demonstrate the effectiveness of incorporating climate change content into pharmacology education and highlight opportunities for broader curriculum development to prepare healthcare professionals with knowledge and skills needs to address challenges related to climate change.
The World Health Organization has identified Climate Change as the greatest threat to public health in the 21st century and a global burden that is impacting the health and well-being of patients across the lifespan in multiple health domains (World Health Organization, 2023). Climate change exacerbates public health challenges through wildfires, heat waves, vector borne disease, medication shortages, and other major events (Smith, et al., 2023, Parums, 2024;). Poor air quality, flooding, and sanitation issues further increase the risks of heat-related illnesses, respiratory and cardiovascular conditions, and waterborne diseases (Smith, et al., 2023).
The increasing intensity and frequency of these issues directly impact human health, strain public health systems, and contribute to the global burden of both infectious and noncommunicable diseases (Parums, 2024). Climate change’s impacts on human health is further complicated by the many social determinants of health, as the health of many rural and low-income populations across the globe are expected to be disproportionately impacted by climate change (Ragavan, et al., 2020; Smith, et al., 2023; Environmental Protection Agency, 2024; Parums, 2024). Additionally, the global healthcare system itself is a significant contributor to greenhouse gas (GHG) emissions and is responsible for approximately 5% of GHG emissions globally (Or, 2024).
Healthcare professionals (HCPs) are in a prime position to raise awareness of the implications of climate change for patient care and to address the impacts of climate change on patient health, and therefore require sufficient knowledge and tools to fulfil this role (Kreslake et al., 2018; Sorensen et al., 2024). For instance, resources are available to guide HCPs in diagnosis and treatment of heat-related illness (HRI), and to educate HCPs on understanding how select medications may increase the risk of HRI through known and theoretical drug mechanisms (Mueller et al., 2024).
International organizations such as the Global Consortium on Climate and Health Education (GCCHE) have recommended integrating climate change into HCP curricula (Sorensen et al., 2023); within the nursing profession, organizations including The International Council of Nurses (ICN) have called for immediate action from governments, health system leaders, and educators to combat climate change and to care for affected people of climate change across the globe (ICN). To support these efforts, organizations such as GCCHE and the Consortium of Universities for Global Health have developed educational frameworks such as the Climate Resources for Health Education initiative and compiled other educational resources like the Planetary Health Report Card to support integration of climate change into HCP curricula.
Despite these initiatives, there has been insufficient progress in integration of climate change education into HCP curricula and continuing education (Sorensen et al, 2023). The authors conducted a targeted literature search and identified a limited number of studies addressing the integration of sustainability and climate change within advanced pharmacology courses for post-licensure nursing programs. This gap in literature supported the development of this pilot study, whose purpose was to evaluate the impact of integrating a single, one-hour climate change education module into an advanced pharmacology course on APRN students’ knowledge and attitudes related to climate change and sustainability within healthcare using pre-and post-lecture surveys.
Description of the Innovation – Guided by a targeted literature review, faculty developed a conceptual model to support the integration of climate change principles into pharmacology education for APRNs, emphasizing the bidirectional relationship between climate change, pharmaceutics, and prescribing patterns.
These relationships are bidirectional. For example, climate change is contributing to a rise in respiratory illness, which has led to the increased use of rescue inhalers and other inhaler therapies (Gupta et al., 2024). Conversely, the prescribing and use of medications, such a pressurized metered dose inhalers (pMDI) to treat these conditions, contribute to climate change through their production, use, and disposal. In fact, the greenhouse gas emissions from one single pMDI inhaler are comparable to driving 180 miles (Fidler et al, 2022). This bidirectional approach highlights a feedback loop where clinical decisions are both influenced by and contribute to planetary health outcomes.
Students were provided with 1) an optional pre-lecture assessment; 2) a one-hour lecture that introduced the new climate change model and its application to major diseases and conditions impacted by climate change including respiratory illness, HRI, and vector-borne diseases; and 3) an optional post-lecture assessment designed to measure changes in attitude and knowledge of climate change and pharmacology. This module was integrated into the Spring semester 2023 Advanced Pharmacology Across the Life Span course for APRN students.
Instrument – The identical pre-lecture and post-lecture assessment consisted of two parts:
Attitude Assessment: SANS-2 Survey
The SANS-2 survey evaluates nursing student attitudes toward climate change, sustainability, and integration of these concepts into nursing curricula, and has been previously studied in undergraduate and graduate nursing students and demonstrated good internal consistency (Richardson et. al, 2019). We adapted 4 of the 5 questions from the survey, and responses were required using a 7-point Likert scale, where 1 = “strongly disagree”, and 7 = “strongly agree”. Faculty received approval from the SANS-2 survey lead author, Janet Richardson, for use of the survey.
Knowledge Assessment: Multiple choice questions and open-ended questions:
A series of knowledge-based questions were developed by the study authors who are faculty within the areas of pharmacology, nursing education, and climate change. The knowledge assessment consisted of four multiple-choice questions. These addressed key lecture content: (1) identifying drug classes that increase sweating/hyperhidrosis, (2) drug classes that decrease sweating/hyperhidrosis, (3) medications associated with photosensitivity, and (4) determining which inhaler types are most environmentally sustainable. Questions were designed to assess students’ understanding of pharmacologic principles in the context of climate-related health risks.
Statistical Analysis – Pre-lecture and post-lecture survey responses were analyzed to evaluate changes in student knowledge and attitudes. Knowledge question responses were compared using McNemar’s test for paired categorical data, with odds ratios (OR) and 95% confidence intervals (CI) reported. Responses to the seven-point Likert scale measuring attitudes towards climate change were summarized using medians and interquartile ranges (IQRs). Changes between pre- and post-lecture attitudes were analyzed using the Wilcoxon rank-sum test, and effect sizes (r) were calculated using only complete pairs. All significance levels were set to a p <0.05.
Ethical Approval – This project was reviewed by the Institutional Review Board at Emory University and was classified as exempt. To ensure further protection for participants, course faculty did not include completion of this lecture evaluation in the formal grading requirements for the course.
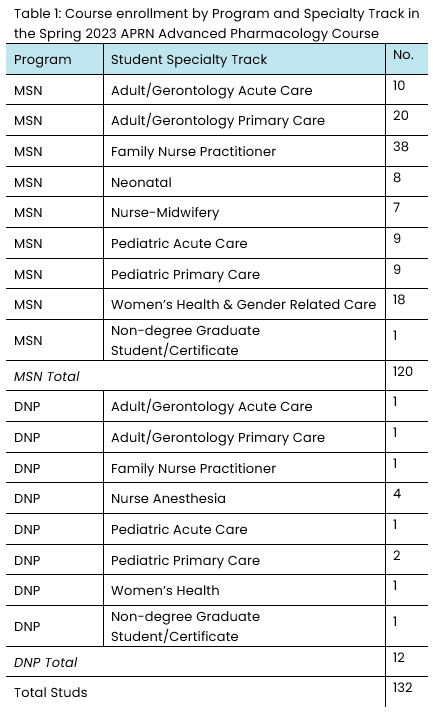
Demographics – Student demographics are shown in Table 1. One hundred and thirty-two students were enrolled in the course (120 Master of Science in Nursing [MSN], 12 Doctor of Nursing Practice [DNP]). Out of the total possible sample, 57 (43%) participated in the pre-lecture survey and 41 (31%) participated in the post lecture survey.
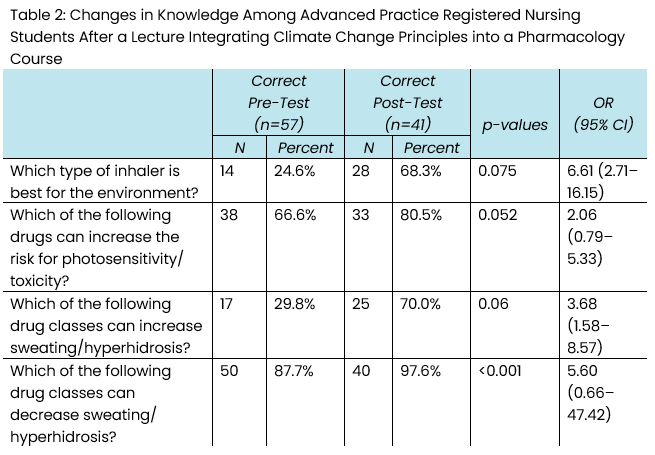
Knowledge – The results of the knowledge questions are shown in Table 2. The proportion of students correctly identifying which drug classes decrease sweating/hyperhidrosis significantly increased from 87.7% to 97.6% (p<0.001). While increases in knowledge were observed for identifying the most environmentally friendly inhaler, drug classes increasing photosensitivity, and drug classes associated with increased sweating/hyperhidrosis, these results did not reach statistical significance.
Despite improved overall performance, over 30% of students continued to answer certain concept-based knowledge questions incorrectly. Specifically, the pre-lecture question on identifying the most environmentally friendly inhaler had a post-lecture to 68.3%, and the item assessing knowledge of drug classes associated with increased sweating/hyperhidrosis was answered correctly by only 70.0% post-lecture. These findings suggest that several concepts from the module may require additional reinforcement or repetition throughout the semester.
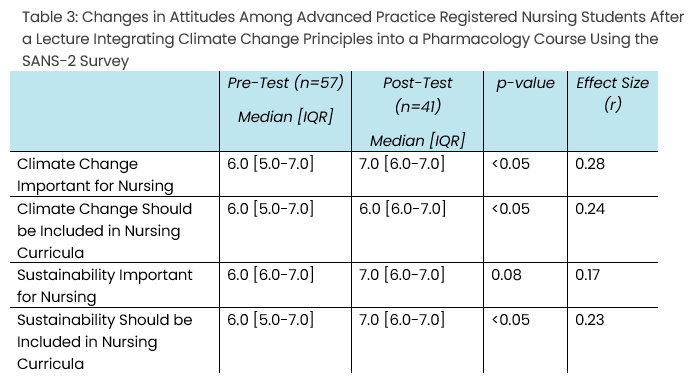
Attitudes –Changes in the students’ attitudes are shown in Table 3. Significant improvements were observed in students’ agreement with the importance of climate change for nursing (p<0.05), the inclusion of climate change in nursing curricula (p<0.05), and the inclusion of sustainability in nursing curricula (p<0.05). While the median score for the importance of sustainability in nursing increased, this change was not statistically significant.
This study builds upon current literature supporting integrating climate change into HCP curricula. Prior studies have demonstrated that even short, single module interventions can enhance student attitude and knowledge on climate change and sustainability within nursing programs (Álvarez-Nieto et al., 2024). Our findings indicate that integration of climate change content into an advanced pharmacology course for APRN students positively impacted their attitudes and knowledge regarding climate change. Statistical significance was observed with three of the SANS-2 attitude survey questions. While only one knowledge-based question achieved statistical significance, improvements were seen with the other knowledge-based multiple-choice questions as well.
This study had several limitations. First, while several attitude-based questions had statistically significant improvements, the improvement from 6 to 7 on the Likert scale may have limited significance. The pre- and post-lecture assessments were optional, and it is possible that students with interest in climate change or pharmacology may have been more likely to participate. Additionally, the small sample size, resulting from response rates of 43% for the pre-lecture survey and 31% for the post-lecture survey, was a limitation. A higher response rate may have increased the power of the study, potentially enabling statistical significance across all knowledge- and attitude-based questions. Another limitation was the design of the knowledge-based questions, which were primarily designed by faculty as multiple-choice and open-ended questions. Future validation of student knowledge could incorporate a combination of formative assignments with application of the climate change model through case studies, essays, and group presentations.
While the overall improvement in student knowledge was positive, there was variability across individual knowledge items, with over 30% of students missing certain concept-based questions. Several factors may have contributed to the learning variability. First, the lecture content was delivered as a single stand-alone lecture offered midway through the semester. This single exposure may not have allowed adequate time for learning, reinforcement, and retention of new concepts.
Future course designs could include longitudinal reinforcement with early introduction of the climate change model to allow for integration and application throughout the semester. Evidence based strategies such as spaced repetition and cased based multiple-choice questions have been shown to support improved learning and retention (Price et al., 2025). Embedding the climate change model across multiple lectures or courses with periodic follow up assessments may encourage sustained knowledge retention over time.
Currently, faculty are conducting a scoping review to further demonstrate the gap in knowledge of the bidirectional relationship of prescribing patterns, pharmaceutics, and climate change within the proposed climate change model, as well as the adaptability of the climate change model for all HCP curricula. Future plans include assessment of knowledge and attitudes toward climate change and sustainability amongst a variety of HCP learners, with the goal of implementing the climate change model broadly within HCP education.
Despite the multiple limitations, this small pilot study demonstrated improvement in APRN students’ knowledge and attitudes towards climate change and sustainability within healthcare. Expanding climate change education across all HCP curricula is critical to preparing future HCPs to address the growing healthcare challenges stressed by climate change. Continued research in providing educational frameworks and models that can be seamlessly applied amongst all HCPs is essential in preparing the next generation of HCPs to address climate change.
In summary, incorporation of climate change content into an advanced pharmacology course for APRNs can positively change nursing student attitudes towards the importance of climate change and sustainability. Climate change curricula should be interwoven amongst all courses of HCP education.
The authors are grateful to the Woodruff Health Educators Academy (WHEA) Fellowship in Educational Scholarship small group leaders, Bruce Greenfield and Dheepa Sekhar, for their support in navigating the WHEA fellowship. Additionally, we are grateful for Rachel Nash who helped with the IRB process, Janet Richardson who granted approval of the SANS-2 survey, and Laura Kimble in providing professional mentorship. We received no grant support for this work. The authors declare that we received no payment or services from any third party to support this work.
Álvarez-Nieto, C., Parra-Anguita, L., Álvarez-García, C., Montoro Ramirez, E.M., López-Franco, M.D., Sanz-Martos, S., & López Medina, I.M. (2024). Sustainability education in nursing degree for climate-smart healthcare: A quasi-experimental study. International Journal of Sustainability in Higher Education, 25(9), 278-292. https://doi.org/10.1108/IJSHE-01-2024-0061
Environmental Protection Agency. (2024, November). Climate change and the health of socially vulnerable people. https://www.epa.gov/climateimpacts/climate-change-and-health-socially-vulnerable-people
Fidler, L., Green, S., & Wintemute, K. (2022). Pressurized metered-dose inhalers and their impact on climate change. Canadian Medical Association Journal, 194(12), E460-E460. https://doi.org/10.1503/cmaj.211747
Global Consortium on Climate and Health Education. (2018). Core climate & health competencies for health professionals. Columbia Mailman School of Public Health. https://www.publichealth.columbia.edu/research/centers/global-consortium-climate-health-education/core-competencies
Gupta, S., Couillard, S., Digby, G., Tse, S. M., Green, S., & Penz, E. (2024). Climate change and inhaler selection in patients with respiratory disease. Chest, 165(3), 503-6. https://doi.org/10.1016/j.chest.2023.09.025
International Council of Nurses. (2018, September). International Council of Nurses calls for increased nursing leadership to combat effects of climate change on health. https://www.icn.ch/news/international-council-nurses-calls-increased-nursing-leadership-combat-effects-climate-change
Kreslake, J.M, Sarfaty, M., Roser-Renouf, C., Leiserowitz, A.A., & Maibach, E.W. (2018). The critical roles of health professionals in climate change prevention and preparedness. American Journal of Public Health, 108(S2):S68-S69. https://doi.org/10.2105/AJPH.2017.304044
Mueller, K., Allstrom, H., Smith, D.J., Downes, E., & Modly, L.A. (2024). Climate change’s implications for practice: Pharmacologic considerations of heat-related illness. The Nurse Practitioner, 49(10):30-38. https://doi.org/10.1097/01.NPR.0000000000000230
Or, Z., & Seppänen, A. V. (2024). The role of the health sector in tackling climate change: A narrative review. Health Policy, 143,105053. https://doi.org/10.1016/j.healthpol.2024.105053
Parums, D.V. (2024). A review of the increasing global impact of climate change on human health and approaches to medical preparedness. Medical Science Monitor, 30. https://doi.org/10.12659/MSM.945763
Price, D. W., Wang, T., O’Neill, T. R., Morgan, Z. J., Chodavarapu, P., Bazemore, A., … & Newton, W. P. (2024). The Effect of Spaced Repetition on Learning and Knowledge Transfer in a Large Cohort of Practicing Physicians. Academic Medicine, 10-1097. https://doi.org/10.1097/ACM.0000000000005856
Ragavan, M.I., Marcil, L.E., & Garg, A. (2020). Climate change as a social determinant of health. Pediatrics, 145(5), e20193169. https://doi.org/10.1542/peds.2019-3169
Richardson, J., Clarke, D., Grose, J., & Warwick, P. (2019). A cohort study of sustainability education in nursing. International Journal of Sustainability in Higher Education, 20(4), 747-760. https://doi.org/10.1108/IJSHE-02-2019-0064
Smith, D. J., Mizelle, E., Leslie, S. L., Li, G. X., Stone, S., Stauffer, P., Smith, A., Lewis, G., Rodden, E. L., McDermott-Levy, R., & Thompson, L. M. (2023). Intervention studies to reduce the impact of climate change on health in rural communities in the United States: A systematic review. Environmental Research: Health, 1(3), 032001. https://doi.org/10.1088/2752-5309/acbbe6
Sorensen, C., Campbell, H., Depoux, A., Finkel, M., Gilden, R., Hadley, K., Haine, D. Mantilla, G., McDermott-Levy, R., Potter, T. M., Sack, T. L., Tun, S., & Wellbery, C. (2023). Core competencies to prepare health professionals to respond to the climate crisis. PLOS Climate 2(6): e0000230. https://doi.org/10.1371/journal.pclm.0000230
Sorensen, C.J., & Fried, L.P (2024). Defining Roles and responsibilities of the health workforce to respond to the climate crisis. Journal American Medical Association Network Open, 7(3): e241435. https://doi.org/10.1001/jamanetworkopen.2024.1435
World Health Organization. (2023, September). Climate Change. https://www.who.int/news-room/fact-sheets/detail/climate-change-and-health
Senior Clinical Instructor, Nell Hodgson Woodruff School of Nursing, Emory University
https://orcid.org/0009-0007-8920-3208
Assistant Clinical Professor, Nell Hodgson Woodruff School of Nursing, Emory University
https://orcid.org/0000-0003-2208-3399
Assistant Professor, University at Buffalo Nursing School
https://orcid.org/0000-0003-4471-8885
Published: 7/21/25