Interactive, interdisciplinary workshops can effectively introduce climate and environmental justice topics into health professions education, fostering knowledge and skills crucial for addressing health inequities in clinical practice.
Introduction: Climate change exacerbates health inequities and environmental injustices. Gaps persist in formal medical curricula addressing the implications of climate change for health and health equity. Emory University’s longitudinal Climate Change and Environmental Health thread, in collaboration with the Community Learning and Social Medicine course, developed and implemented an interactive, multidisciplinary workshop designed to introduce first-year medical students to the foundational principles of climate and environmental justice.
Methods: First-year medical students from the class of 2028 participated in a two-hour interactive workshop on environmental justice, focusing on its implications for clinical practice and interdisciplinary collaboration. The workshop, co-created by students, faculty, and staff, included four interactive sessions covering topics such as planetary health, redlining and urban heat, Indigenous knowledge, and food justice. Participant attitudes toward the workshop were assessed using an online post-workshop survey.
Results: A total of 142 out of 150 first-year medical students (95%) participated in this environmental justice workshop, with 72 (51%) completing the post-workshop evaluation. Among respondents, the vast majority (90%) agreed that physicians have a role in addressing climate and environmental health needs, and 72% reported that the workshop improved their knowledge, skills, and attitudes relevant to patient care. Interactive, interdisciplinary approaches were highlighted as particularly valuable, though some students expressed a desire for deeper clinical application.
Conclusions: The workshop demonstrated feasibility, acceptability, and effectiveness in enhancing medical students’ engagement with climate and environmental justice. Future efforts will focus on expanding clinical applications and longitudinal assessments.
Human health depends on access to clean water, clean air, healthy food, and safe environments. Climate change impinges upon these basic needs, posing dire consequences for health and healthcare systems (Hayden et al., 2023). Environmental Justice (EJ) describes the inequitable impacts of the environment, many of which are interconnected with climate change, on diverse groups of people. (Resnik, 2022). Many EJ challenges are rooted in the unsustainable consumption of natural resources, including fossil fuels. Harmful exposures, from industrial waste and byproducts to traffic-related air pollution, are often concentrated in specific geographic areas, in part due to structural discrimination, defined as policies, cultural norms, and institutional practices that perpetuate inequality and disadvantage for specific groups (Romanello et al., 2022). Knowledge of not only the medical consequences of environmental exposures, but also their structural underpinnings, will better equip physicians to tailor patient-centered anticipatory guidance, preventive care, and treatment plans, and to forge connections with community resources.
The National Academy of Sciences, Engineering, and Medicine (NASEM) emphasized a gap in training on the environment as a determinate of health decades ago (Institute of Medicine Committee on Curriculum Development in Environmental, 1995). More recently the NASEM, the Association of American Medical Colleges, and other prominent institutions have called attention to the consequences of the climate crisis for health and health equity. Many physicians and educators lack formal training on climate change and health. In contrast, almost 75% of Emory Medical School’s class of 2028 received formal curricula on climate change and/or environmental health in high school or earlier based on a poll of first year students in 2024. The same poll revealed, however, that more than 10% of the class had not received any formal education on the topic prior to matriculation.
While students enter medical school with vast differences in knowledge and lived experience around climate and health, many are keenly interested in this topic. In 2020, a group of Emory medical students founded Medical Students for Climate Action (MSCA), with three pillars of engagement: EJ, medical education, and healthcare sustainability. MSCA students and faculty co-created a curriculum that interweaves Climate Change and Environmental Health (CCEH) with existing medical school courses (Rabin, Laney, & Philipsborn, 2020). Initiated as a grassroots pre-clinical curriculum, this effort was formalized in 2022 as the CCEH thread with plans to span all four years of medical education.
A medical student focus-group evaluating Emory’s CCEH curriculum identified continued focus on EJ, collaboration with longitudinal courses, and interactive sessions as priorities (Liu, Rabin, Manivannan, Laney, & Philipsborn, 2022). Emory’s longitudinal Community Learning and Social Medicine (CLSM) course, focused on increasing students’ understanding of the social determinants of health, presented an opportunity for partnership with the CCEH thread on an EJ workshop. Practically speaking, incoming students needed a foundation upon which to build their knowledge, skills, and attitudes related to climate change and environmental health over the four years of medical education. They also needed to understand the environment as a major determinate of health in order to contextualize the content of their early physiology- and pathology-focused courses and be prepared to apply this knowledge to patient care in their clinical clerkship years. To that end, the CLSM Course and CCEH thread teamed up to create, implement, and evaluate a workshop on climate and environmental justice.
Description of the Innovation
First year medical students from the class of 2028 participated in a two-hour interactive workshop on EJ with an emphasis on implications for clinical practice and interdisciplinary collaboration. This novel, interactive session was introduced into a longitudinal, community-based curriculum by CLSM and the CCEH thread. The implementation team included six faculty educators (5 from the MD program with specialties including Internal Medicine, Pediatrics, and Emergency Medicine, and one from the Physician Assistant program), two staff members (from Emory’s Turner Environmental Law Clinic and Rollins School of Public Health), and five students. Transcending roles to co-create this workshop, the implementation team members were united by their interest in how social structures can promote or detract from individual health. Most of the student members had previously participated in co-creation efforts with the CCEH Thread.
During the workshop, students rotated between four sessions (25 minutes each) in groups of approximately 35. Topics were selected to build a foundation of knowledge focused on climate change as a force that compounds the existing challenges of the structural determinants of health. Each session emphasized opportunities for physicians to support health and health equity by embracing the health benefits of planetary health approaches. Planetary health is a concept that acknowledges the interdependence of human health and the environment, including the natural resources on which life depends (Whitmee et al., 2015). Planetary health approaches often transcend disciplines, emphasizing collaborative solutions and cultural humility. In each session, the theme of cultural humility, a process of reflection and curiosity in understanding the values and experiences of others, was explored in relation to patient-centered care. Facilitators were equipped with materials to implement their sessions. Slide decks for each session included learning points and key figures. Facilitators shared the overall workshop objectives with the first group and subsequently presented their session’s learning points (Box 1).
Box 1: Session objectives for a novel environmental justice workshop for first year medical students | ||
Overall Environmental Justice Workshop Objectives | ||
Conceptualize climate change as a “threat multiplier” for populations already at risk of health inequities and environmental harms Identify synergies between climate justice and your professional identity formation as physicians Practice “cultural humility” with an environmental justice lens in clinical encounters Build a foundation on which to integrate climate change into your framework of learning over the next 4+ years | ||
Session Learning Points | ||
Foundations of Climate Change and Environmental Justice | Define “planetary health” and state in your own words why climate change matters for medicine. Identify 3 ways that climate change disrupts healthcare delivery (e.g. direct impact on facility operations, disruption of supply chains, displace patients from your medical homes during regional disaster scenarios). | |
Redlining, Urban Heat, and Environmental Justice in Practice | Recognize redlining as an example of structural racism that results in health disparities via disproportionate exposure to environmental and other harms. Learn from interprofessional colleagues: what are opportunities for the clinician and clinical care to better assess and address environmental exposures that matter to our patients and local communities. Collaborate across disciplines to identify and access resources to help address patient and community environmental health problems and concerns. | |
Planetary Health and Indigenous Knowledge | Engage with Indigenous conceptualizations of planetary health with cultural humility and respect. State the approximate percent contribution of the US Healthcare Sector to US greenhouse gas emissions. Chart intersections between Indigenous leaders’ planetary determinates of health in the article and current health care delivery. | |
Food, Child Rights and Intergenerational Justice | Articulate the ethical implications of climate change for human rights as well as social and intergenerational justice. Explore how US dietary patterns contribute disproportionately to the health harms of climate change and ways in which physicians support children in confronting this system. | |
Session 1: Foundations of Climate Change and Environmental Justice
For this portion of the workshop, student facilitators reviewed brief slides showing the basics of planetary health and climate justice. Students then broke into small groups to answer key questions about climate change (one per group) and share their responses with the large group. The prompts were: 1) Why is climate change happening and what are the biggest contributors to climate change; 2) When will we see the consequence of climate change; 3) How long do we have to mitigate emissions to avoid the consequences of climate change that are potentially catastrophic and irreversible; 4) Where will climate impacts be felt the most; and 5) Who is most at risk for negative climate-health impacts? As students shared findings with the group, the facilitator presented slides with graphics matched to each question. At the conclusion of the session, the facilitator introduced an interactive tool that explores how climate change affects patient health and the practice of medicine across medical specialties and organ systems, as well as approaches to consider these implications for clinical practice (Salas & Solomon, 2019).
Session 2: Redlining, Urban Heat, and Environmental Justice in Practice
In this session, public health and law professionals presented students with cutting edge research on heat and health as well as community resources to support clinical practice. The Emory Climate and Health Actionable Research and Translation (CHART) Center is developing ways to better characterize and address health risks of extreme heat on under-resourced communities, including formerly redlined communities, defined as those whose residents were historically denied financial services based on their racial or ethnic composition. As part of this project, the CHART team is developing questionnaires and working with electronic medical record data to understand patient-level risk and protective factors surrounding heat illness in the local community. Students worked with a facilitator to brainstorm clinically-relevant questions to assess a patient’s vulnerability to extreme heat. Finally, legal staff from the Turner Environmental Law Clinic presented information about the Environmental Justice Green Book, an online resource designed to empower communities facing environmental injustices in Georgia (“Environmental Justice Green Book for Georgia,” 2023). The EJ Green Book includes explanations of environmental laws, a list of strategies, legal templates, and resources, and a database of environmental justice organizations, government agencies, and community-based initiatives in Georgia. The presentation focused on the EJ Green Book as a resource for medical students, health providers, and community members.
Session 3: Planetary Health and Indigenous Knowledge
In this session, faculty and student facilitators reviewed key aspects of Indigenous stewardship of the planet in contrast with our healthcare system’s unsustainable consumption of resources. The session reviewed: 1) key points of Indigenous stewardship of planetary resources, 2) the percent contribution of the US healthcare sector to global greenhouse gas emissions, and 3) tools from the Joint Commission, the organization that accredits US hospitals, and NASEM to further sustainability efforts. Students participated in a collaborative activity where they read one of 10 planetary determinates of health with a small group (Redvers et al., 2022) and then discussed these questions: 1) What are specific gaps between current healthcare delivery and the more holistic vision of health proposed in the article; and 2) What are potential paths forward or solutions to bridge these gaps? Then, the students came back together as a large group and shared their ideas and reflections.
Session 4: Food, Child Rights, and Intergenerational Justice
For this part of the workshop, faculty and student facilitators introduced diet as one of the most powerful levers both to reduce global greenhouse gas emissions and to improve health (Hawken, 2017; Swinburn et al, 2019). Many physicians, especially in the outpatient clinical setting, already engage patients routinely about diet and nutrition (Swinburn, et al., 2019). Three slides covered key facts about 1) current diets in the US and the degree to which they exceed planetary health bounds, 2) the health and planetary health benefits of eating less meat, and 3) the changing dietary patterns in the US (Willett et al., 2019). Students then critically observed a role-play of dietary counseling with many opportunities for improvement. Students suggested ways to deliver more patient-centered counseling which were then adopted in a second, more patient-centered role-play of clinician-patient dietary counseling that also applied principles of planetary health.
Session Evaluation – All students were provided with a QR code link to an anonymous evaluation and asked to complete it before leaving. Evaluations were accepted up to 1.5 hours after the conclusion of the workshop. The evaluation assessed students’ perceptions of how the workshop contributed to their ability to care for patients affected by climate change or EJ concerns. Questions asked for students’ perception of the workshop’s contribution to their relevant knowledge, skills, and attitudes, their cultural humility, and their understanding of the role of interprofessional collaboration in caring for patients with EJ concerns. The evaluation also included questions about students’ expectations for learning about CCEH in medical school as well as their beliefs regarding the role of physicians in addressing CCEH concerns as a part of their clinical practice. Response options for all questions were a 5-point Likert scale from strongly agree to strongly disagree. Two final open-ended questions elicited student perspectives on strengths and opportunities for improvement of the workshop
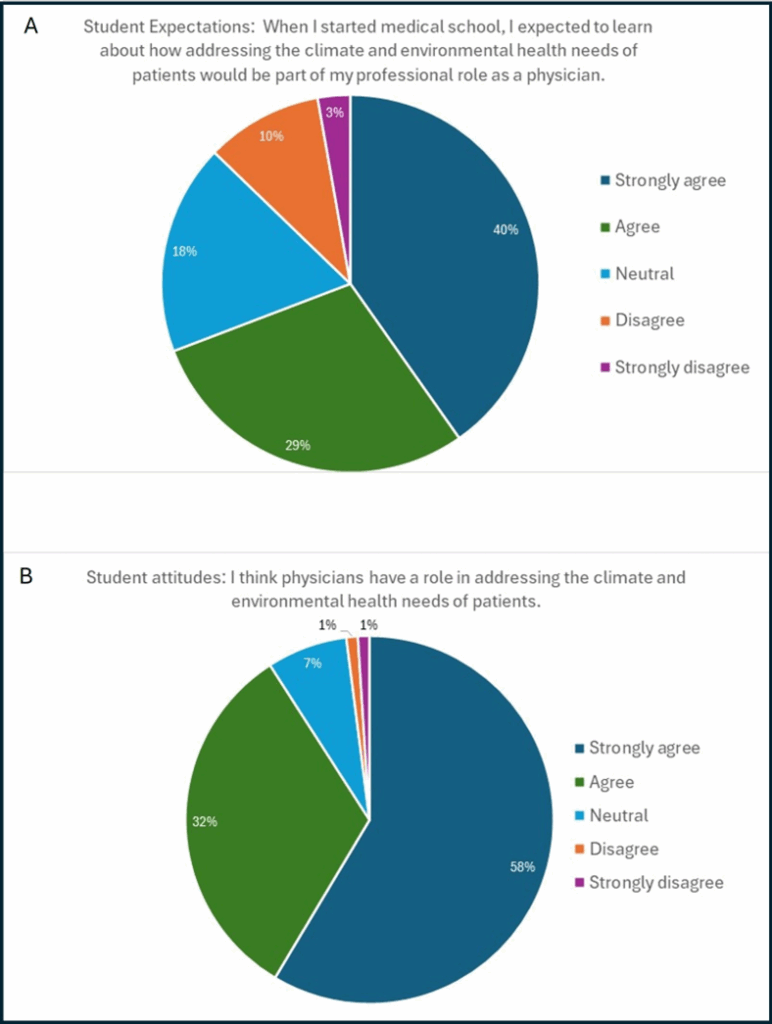
One hundred forty-two (95%) of 150 first year medical students participated in the workshop. Of the 142 students who attended the workshop, 51% completed the full evaluation (N=72). Fifty of these 72 students (69%) agreed that when they started medical school they expected to learn about how addressing the climate and environmental health needs of patients would be part of their professional role, and sixty-five (90%) agreed that physicians have a role in addressing the climate and environmental health needs of patients (Fig 1).
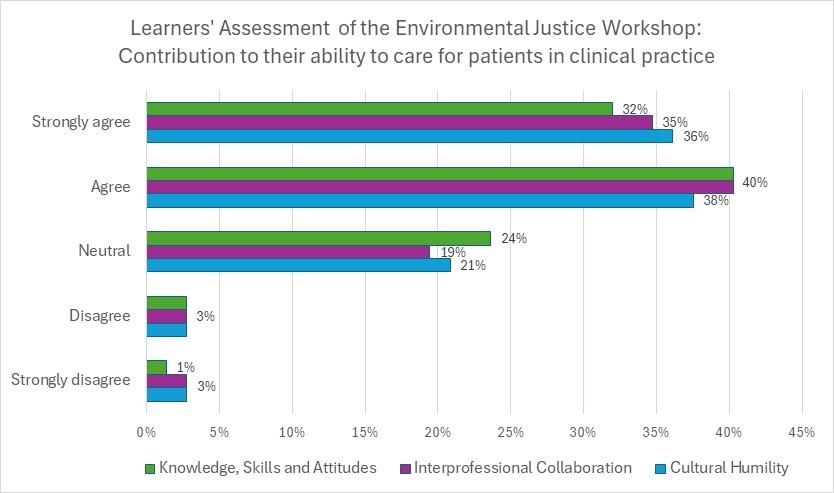
When assessing whether the workshop prepared them to meet the needs of patients with climate or environmental justice concerns in clinical practice: 52 (72%) of respondents agreed that the workshop helped them develop relevant knowledge, skills, or attitudes, 54 (75%) agreed that the workshop helped them understand the role of interprofessional collaboration, and 53 (74%) agreed that the workshop helped inform their cultural humility (Fig 2). No more than 4 students (6%) disagreed with any of those statements.
Nineteen students wrote open-ended general comments on the workshops. Students generally appreciated the discussions, attention to cultural humility, and the interactive nature of the sessions. Some requested even more discussion, interaction and clinical application across the sessions, suggesting more case studies (especially examples of engaging law and public health).
For example, one student would have liked to see, “More specific examples of how climate change is impacting individuals… examples of the harm of healthcare on individuals, or potential solutions in the works.” Other students would have liked the workshop to facilitate engagement with the surrounding community or advocacy, with one stating: “I love these sessions! They were so informative but I’m wondering if instead [of] us learning about it: I wonder if we can use the knowledge to teach them to surrounding communities. I think doing something more active would be wonderful like going to a hearing or showing up to a house legislature session when they are deciding on a climate law or food policy.”
This EJ workshop for first year medical students emphasized collaborative learning, patient-centered approaches, and the development of cultural humility in addressing environmental determinants of health. The workshop was feasible to implement, acceptable to students, and effective in enhancing students’ self-reported knowledge, skills, and attitudes related to climate change and EJ. Students overwhelmingly believe that physicians have a role in addressing climate change and environmental health challenges faced by patients – an inspiring contrast with healthcare’s status quo. While most indicated that the workshop helped prepare them for climate and EJ concerns in clinical practice, about a quarter of the class responded more tepidly – suggesting room for future improvement. Future iterations could benefit from even more space for discussion and interaction, an opportunity for more participant-engaged teaching, inclusion of more clinical cases that emphasize the role of the physician in working with interprofessional colleagues (for example, public health or applied health-environmental law), or environmental justice case studies or solutions in the healthcare sector.
This workshop–created by an interprofessional team and with sessions emphasizing collaboration–provided medical students with early exposure to the ways in which physicians work with other professionals when caring for patients. While it was not feasible for this workshop to include learners from other health professional schools, engaging diverse professional perspectives in the design and implementation of the workshop enhanced the content and its delivery. Modeling and introducing inclusive practices early in the medical curriculum could enhance students’ aptitude for engaging different viewpoints in clinical settings. This approach offers a valuable model for other programs aiming to incorporate interprofessional perspectives into the application of CCEH content. In addition, planetary health frameworks emphasize interconnectedness and sustainability—principles often absent from healthcare discourse. By fostering dialogue that includes these perspectives, medical education may promote more holistic approaches to patient care.
Our evaluation has limitations. Only about half of students responded to the survey, introducing the potential for response bias. The evaluation elicits learners’ perceptions of their learning outcomes rather than objective measures of student knowledge, skills, and attitudes after the workshop. The overall evaluation would be strengthened by including perspectives from the implementation team as well. Finally, the evaluation questions are not validated tools. Nevertheless, these modest data provide valuable insight in designing future iterations of the workshop.
Some of our opportunities for improvement are related to the wide range of incoming knowledge of first year medical students. As students increasingly enter medical school with prior knowledge of climate change and EJ, the curriculum must be continually revised. Facilitators must strike a balance between providing a foundation for those who are new to the content while supporting in-depth engagement for students with more experience – both lived and academic. While pre-clinical students embrace the role of physicians in addressing CCEH challenges in clinical care, they are still inexperienced in clinical practice. This dissonance underscores an opportunity to further integrate environmental health content into the clinical skills portion of the pre-clinical curriculum.
Future efforts will focus on expanding longitudinal assessments to track the integration of climate justice principles into professional identity formation. This early workshop presents an opportunity to introduce a post-workshop objective assessment and repeat this assessment later in the curriculum to evaluate decay in knowledge, skills, or attitudes related to EJ. We will continue professional development activities to ensure that students are supported in practicing the principles from this workshop in clinical learning environments. Finally, CCEH and CLSM faculty and students hope to expand opportunities for community engaged coursework. Ultimately, this inclusive and collaborative workshop strives to equip future physicians to tackle complex health challenges and foster innovative strategies that bridge gaps between current practices and sustainable, community-centered care.
The intersection of climate change, EJ, and health is increasingly recognized as essential for improving patient and community health outcomes. Curricula on EJ can help equip future physicians and other health professionals with the knowledge and skills necessary to address these critical issues throughout their training.
Dr. Philipsborn would like to acknowledge support from the Josiah Macy Jr Foundation that has helped to support this work. The authors received no other grant support for this work and declare they have no conflicts of interest in regard to this work.
Environmental Justice Green Book for Georgia. (2023). Environmental Justice Green Book for Georgia. https://ejgreenbook.com/
Hawken, P. (Ed.). (2017). Drawdown: The most comprehensive plan ever proposed to reverse global warming (1 online resource).
Hayden, M. H., Schramm, P. J., Beard, C. B., Bell, J. E., Bernstein, A. S., Bieniek-Tobasco, A., … Wilhelmi, O. V. (2023). Human health. In A. R. Crimmins, C. W. Avery, D. R. Easterling, K. E. Kunkel, B. C. Stewart, & T. K. Maycock (Eds.), Fifth National Climate Assessment. U.S. Global Change Research Program.
Institute of Medicine Committee on Curriculum Development in Environmental Medicine. (1995). In A. M. Pope & D. P. Rall (Eds.), Environmental medicine: Integrating a missing element into medical education. National Academies Press (US).
Liu, I., Rabin, B., Manivannan, M., Laney, E., & Philipsborn, R. (2022). Evaluating strengths and opportunities for a co-created climate change curriculum: Medical student perspectives. Frontiers in Public Health, 10, 1021125. https://doi.org/10.3389/fpubh.rorr.1021125
Rabin, B. M., Laney, E. B., & Philipsborn, R. P. (2020). The unique role of medical students in catalyzing climate change education. Journal of Medical Education and Curricular Development, 7, 2382120520957653. https://doi.org/10.1177/2382120520957653
Redvers, N., Celidwen, Y., Schultz, C., Horn, O., Githaiga, C., Vera, M., … Blondin, B. (2022). The determinants of planetary health: An Indigenous consensus perspective. The Lancet Planetary Health, 6(2), e156–e163. https://doi.org/10.1016/S2542-5196(21)00354-5
Resnik, D. B. (2022). Environmental justice and climate change policies. Bioethics, 36(7), 735–741. https://doi.org/10.1111/bioe.13042
Salas, R. N., & Solomon, C. G. (2019). The climate crisis—Health and care delivery. The New England Journal of Medicine, 381(8), e13. https://doi.org/10.1056/NEJMp1906035
Swinburn, B. A., Kraak, V. I., Allender, S., Atkins, V. J., Baker, P. I., Bogard, J. R., … Dietz, W. H. (2019). The global syndemic of obesity, undernutrition, and climate change: The Lancet Commission report. The Lancet, 393(10173), 791–846. https://doi.org/10.1016/S0140-6736(18)32822-8
Whitmee, S., Haines, A., Beyrer, C., Boltz, F., Capon, A. G., de Souza Dias, B. F., … Yach, D. (2015). Safeguarding human health in the Anthropocene epoch: Report of The Rockefeller Foundation–Lancet Commission on planetary health. The Lancet, 386(10007), 1973–2028. https://doi.org/10.1016/S0140-6736(15)60901-1
Willett, W., Rockström, J., Loken, B., Springmann, M., Lang, T., Vermeulen, S., … Murray, C. J. L. (2019). Food in the Anthropocene: The EAT–Lancet Commission on healthy diets from sustainable food systems. The Lancet, 393(10170), 447–492. https://doi.org/10.1016/S0140-6736(18)31788-4
Associate Professor, Department of Pediatrics and Gangarosa Department of Environmental Health, Emory University School of Medicine and Rollins School of Public Health, ORCID 0000-0002-2843-7509
Medical Student, Emory University School of Medicine
Assistant Professor, Department of Emergency Medicine, Emory University School of Medicine
Associate Professor, Departments of Pediatrics and Emergency Medicine, Emory University School of Medicine
Fellow, Turner Environmental Law Clinic, Emory University School of Law
Assistant Professor, Department of Emergency Medicine, Emory University School of Medicine
Department of Family and Preventive Medicine, Emory University School of Medicine
Associate Professor, Department of Internal Medicine, Emory University School of Medicine
Published: 7/21/25