The clinical years of health professionals’ education provide a unique opportunity to discuss the intersection of climate health and patient care. These topics can be easily integrated into existing didactic content on chronic disease etiology and management.
Climate and environmental health education is increasingly recognized by professional societies and medical schools as an important component of medical education. While students and faculty at Emory School of Medicine effectively integrated planetary health education into a “thread” in the pre-clinical MD curriculum, leadership of this Climate Change and Environmental Health thread identified a lack of content in the clinical clerkships. Given its emphasis on disease prevention and chronic disease management, the thread team identified the Adult Primary Care clerkship as an optimal course for incorporation of planetary health education. Thread and clerkship leaders co-created content that incorporated relevant planetary health educational topics into existing clerkship activities. Students utilized their firsthand experience with the curriculum to identify opportunities to include relevant content and to develop those ideas into Adult Primary Care clerkship activities informed by evidence from the planetary health literature. The clerkship directors reviewed these proposals and provided feedback about feasibility and delivery within the clerkship. Ultimately, the teams incorporated content into two activities: a chronic obstructive pulmonary disease workshop emphasizing the impact of environmental exposures on disease development and the environmental impact of medication inhalers, and a chronic disease management activity emphasizing how plant-forward diets can benefit both patient and planetary health. Clerkship content co-creation with planetary health subject area experts and incorporation of student perspectives allowed for evidence-based content development and rapid and feasible integration into existing clerkship activities.
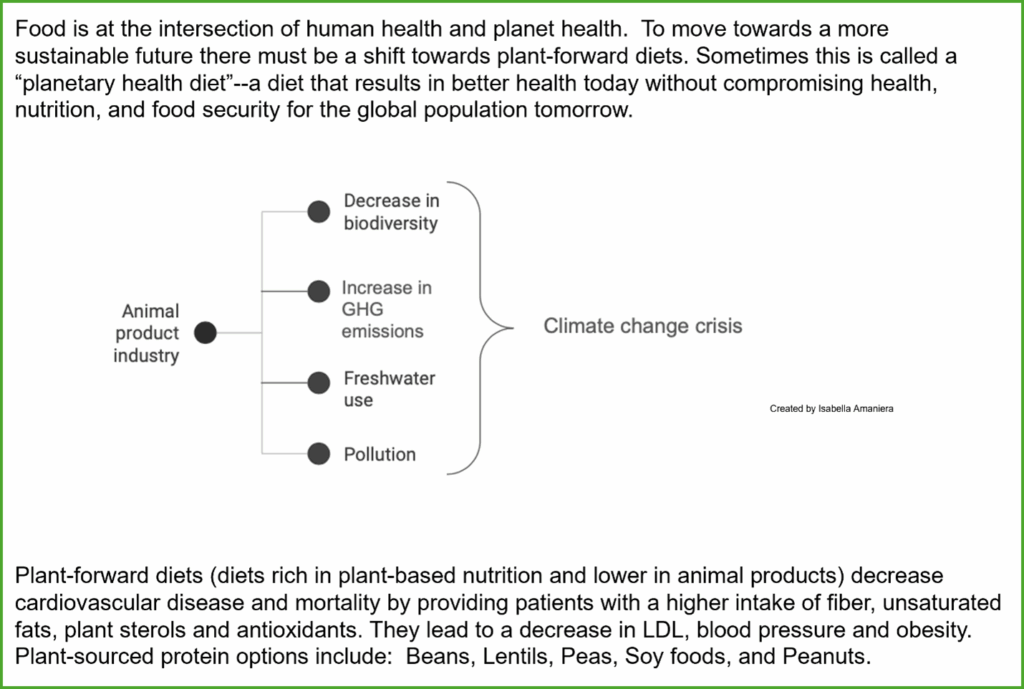
The implications of the climate crisis for health and healthcare delivery are well-described (Romanello et al., 2024; Salas & Solomon, 2019). Many of the actions needed to transform human systems—including the healthcare system—toward a less harmful and more sustainable equilibrium would also improve individual and population health (Gupta et al., 2024; Whitmee et al., 2015). More emphasis on disease prevention in healthcare systems would reduce consumption of resources to treat chronic diseases (Or & Seppänen, 2024). At the same time, healthy diets that consist of more plant-forward components and less meat and processed food than the typical American diet are essential to health promotion and disease prevention and hold profound power in mitigating climate change (Willett et al., 2019). These principles are fundamental to planetary health, a concept defined as the acknowledgement that “the health of human civilization and the state of the natural systems on which it depends” are co-dependent (Whitmee et al., 2015).
Numerous medical professional societies and educational groups have called for the inclusion of climate and health education in medical training, and medical schools are rising to this challenge (Ghosh et al., 2024; Lemery et al., 2024). In a recent Association of American Medical Colleges survey, 70% of medical schools indicated that they include climate and health content in required pre-clinical or clinical courses (Blood A, 2024). In addition, the Planetary Health Report Card (PHRC), a student-driven collaboration that ranks medical school engagement in Planetary Health, scored 53 schools in the United States in 2024 (https://phreportcard.org/wp-content/uploads/2024/04/MEDICINE-PHRC-2024-Summary-Report.pdf).
With its emphasis on prevention and chronic disease management in the outpatient setting, adult primary care education is an optimal venue to incorporate foundational planetary health themes.
Among the early adopters of climate and environmental health education, faculty and students from Emory University School of Medicine embarked on the co-creation of a climate change and environmental health curriculum for medical students in 2019 (Rabin, Laney, & Philipsborn, 2020). The Emory Climate Change and Environmental Health (CCEH) effort initially focused on the eighteen-month pre-clinical, “Foundations” phase within Emory’s four-year MD curriculum. Students and faculty partnered in an intentional co-creation process to identify opportunities to embed CCEH content within existing pre-clinical topics, curate and seamlessly incorporate this content, produce relevant activities, and evaluate the reception of the curriculum (Laney, et al., 2022; Rabin et al., 2020). Showing early promise, the CCEH effort was adopted by Emory’s Executive Curriculum Committee as a formal curricular thread in 2022. As a thread, the CCEH curriculum would be woven through courses and clerkships (required clinical rotations) across all four years of medical education. While the CCEH effort was built with students and involved designated student “curriculum chairs,” the thread designation also provided a formal role for student “thread representatives” for each class.
Despite success in the preclinical realm, the new thread left significant curricular gaps, most notably around the application of CCEH content in clinical clerkships. In a focus group evaluation of strengths and opportunities of the CCEH curriculum, the CCEH team identified expansion to the clinical years and development of clinical skills as a top priority (Liu, et al., 2022). To care for patients in this time of climate crisis, students not only need to acquire knowledge and skills in a classroom setting, but also to apply CCEH concepts to their developing practice of medicine in the clinical learning environment. In addition, the pre-clinical CCEH content, echoing the structure of the pre-clinical curriculum, was focused predominantly on human disease. The clerkship phase of the curriculum offered opportunities to 1) consolidate knowledge and skills on assessing and addressing climate and environmental health risks; 2) emphasize the synergies between an individual patient’s health and planetary health, so-called climate and health co-benefits; and 3) introduce students to their role as clinicians in sustainable care delivery.
While clerkship directors aspire to incorporate new content such as climate health education into their curricula, they may not have the time, expertise, or perspective to implement changes quickly or effectively. Subject matter experts and medical students can bring content-area expertise, teamwork, and learner perspectives to complement the content-delivery and curriculum-building skills of clerkship directors. The tripartite collaboration of Adult Primary Care (APC) clerkship directors, subject matter experts, and students embraced an opportunity to educate students on this highly relevant topic for patient care that was not yet covered in the clinical curriculum. This effort aimed to teach third-year medical students on the APC clerkship the clinical applications of planetary health in the outpatient setting and to encourage them to look for climate-related risk factors, identify patients that are most at risk from climate-related events, and motivate them to consider planetary health when treating common outpatient conditions and discussing their prevention.
The team of a CCEH student representative, CCEH thread director, and APC clerkship leaders applied the co-creation process that the CCEH team used in the pre-clinical phase (Rabin et al., 2020). Having “lived” the curriculum, students identified existing gaps and opportunities in the APC clerkship and presented these to faculty leadership. The CCEH team worked to synergize proposed ideas with evidence from the planetary health literature, existing CCEH content, and the existing APC clerkship activities. The APC team reviewed the proposed ideas in the context of the APC clerkship curriculum, considering potential content areas and didactic sessions that would benefit from and could easily accommodate content about environmental health.
Specifically, the team reviewed content addressing cardiovascular and pulmonary pathology, as air pollution and climate-driven extreme weather clearly affect these conditions, and the CCEH thread provides a foundation for the pathophysiologic basis of these effects in the-preclinical curriculum (Bayram et al., 2023; Kazi et al., 2024; Smirnova, et al., 2023). The team also discussed the intersection of lifestyle management for both personal and planetary health—so-called health co-benefits of climate action— and potential applications to dietary recommendations for chronic disease management (Haines, 2017).
Incorporating these topics in small ways throughout existing sessions or activities in the APC curriculum was straightforward. The clerkship team updates and refines the curriculum annually, and this review process provided an opportunity to incorporate these topics into the existing curriculum. Collaborating with experts in planetary health was essential to rolling out these changes. The CCEH student representative and thread director helped develop the appropriate content that was then integrated into the proper educational sessions by the clerkship leadership team. This integration emphasized the clinical relevance of the climate health content to APC course objectives and materials. Since a variety of educators lead these curricular sessions, APC course leadership placed an emphasis on communicating with session leaders about the content changes to make sure they were familiar with the planetary health topics newly included in their teaching material.
Live Like Your Patient Asynchronous Assignment
The APC clerkship includes the “Live Like Your Patient” exercise, in which students are assigned a chronic health condition (diabetes, hypertension, or chronic kidney disease) and asked to follow a specific diet and mock medication regimen for their condition for two weeks. The existing handouts gave very basic information about dietary restrictions for each condition and links to resources from organizations that could provide more detail. In essence, these handouts were previously a list of foods to eat and those to avoid. The CCEH student representative took the initiative to revamp the handouts, focusing on visual representations of the dietary principles for each assigned chronic illness (Figures 1 & 2).
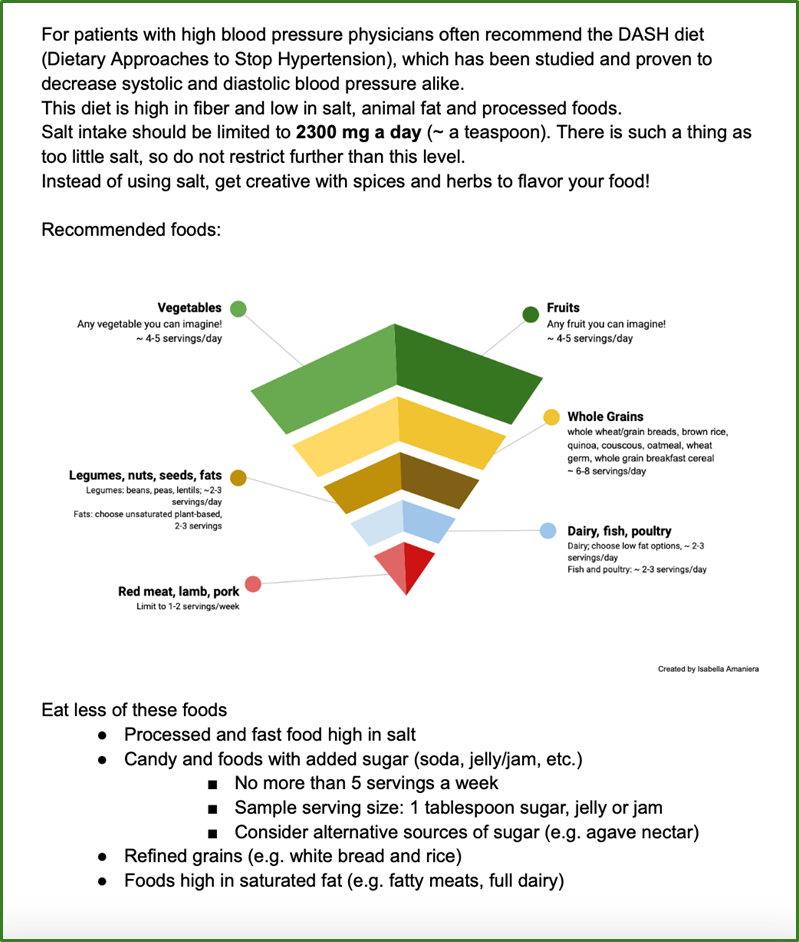
In updating these handouts to be more learner- and patient-friendly, there was an opportunity to highlight elements of the diets that aligned with plant-forward diets and planetary health. While similar to Dietary Approaches to Stop Hypertension (DASH) diets, planetary health diets also emphasize their sustainability and health benefits for patients and the planet (Frank, et. al., 2024). Information was added to the handouts about the impact food has on climate change and how dietary changes that focus on plant-based consumption can improve patient and planetary health as outlined in the EAT-Lancet Commission (Willett et al., 2019). During a group debrief session about the Live Like Your Patient Activity, APC facilitators emphasize how patients can be counseled about planetary health diets in patient-centered, culturally sensitive ways.
COPD Workshop
In addition, the APC clerkship holds a workshop on chronic obstructive pulmonary disease (COPD) diagnosis and management for each group of students. During this experience, students rotate through four stations discussing different components of diagnosis and management of COPD. With the assistance of the CCEH director, the APC team incorporated content about environmental exposures and their impact on the prevalence of COPD into the station about diagnosing COPD, while the environmental impact of different types of medicated inhalers was added to the station about how to use inhalers (Fidler, Green, & Wintemute, 2022).
In order to assess student knowledge and the effectiveness of incorporating planetary health content, the APC clerkship is piloting inclusion of planetary health topics into the existing student assessments and examinations. Currently, some students are assessed on a climate health concept during the APC oral exam, with the goal of future expansion so that all students on the clerkship are assessed on climate health knowledge and application. For the 2025-2026 academic year, the APC clerkship added a debrief element for the Live Like Your Patient activity. In the activity, students write a brief reflection on doctor-patient communication and develop a SMART (Specific, Measurable, Attainable, Realistic, Time-Bound) goal addressing how they plan to better counsel and assist patients in managing their chronic conditions, based on their own experience in following a patient-centered, planetary health diet. Through guided reflection, the goal is to more effectively connect the didactic activities to patient care.
In addition to assessing student climate health knowledge on clerkship-specific assessments, the CCEH thread aims to incorporate climate health knowledge into the Observed Structured Clinical Examination (OSCE) that all students are required to pass after completing their required clerkships. This strategy may provide insight into any decay in learner application of APC-relevant planetary health knowledge, skills, and attitudes since their APC clerkship.
Student performance on assessments will comprise one component of a multi-modal curriculum evaluation approach, supplementing informal and formal strategies. Informal evaluation of the effectiveness of the incorporation of climate health education into the APC clerkship will begin with feedback from students who completed the APC clerkship in the 2024-2025 academic year. Thus far, on routine end-of-clerkship evaluations that are standardized across all clerkships, students have not commented on the climate health education in the APC clerkship. To solicit feedback on this specific area, we will ask the APC clerkship student representative to gather feedback through discussions with classmates and incorporating a planetary health item on an existing voluntary post-clerkship survey. In informal discussions with students, a few have mentioned appreciation of incorporation of climate health content.
To formally evaluate the APC CCEH curriculum, the APC clerkship directors plan to administer a brief student survey specifically about climate health knowledge and attitudes that APC students would complete before and after the COPD workshop and Live Like Your Patient activities. Finally, the CCEH thread may conduct student focus groups to obtain student perspectives on the incorporation of CCEH content in the clinical years, mirroring the pre-clinical focus group strategy.
As students enter the clinical years, opportunities abound to highlight how planetary health impacts common chronic conditions and how the treatments that improve patient health align with those that combat climate change. We have identified additional areas in which we hope to incorporate climate health content on the APC clerkship, particularly in additional education about diet and exercise. For the coming clerkship year, we hope to incorporate more content connecting healthy, plant-based diets with planetary health benefits and the effects of extreme heat from climate change on patient exercise counseling. We also aim to provide students with existing patient handouts that address special considerations for chronic disease management in the climate crisis, including in the context of exposures like extreme heat. These expert-crafted tools emphasize the clinical applicability of this topic and direct patient care component of climate health education.
Additionally, because many clinical preceptors were not exposed to climate health education during their own training, we plan to offer preceptor development sessions on planetary health topics to strengthen their ability to discuss these topics with their students. From a broader curriculum perspective, any other clerkship, program, or school that trains future patient care providers can follow a similar model to partner with CCEH experts to develop and incorporate climate health education into clinical education and training.
Bayram, H., Rice, M. B., Abdalati, W., Akpinar Elci, M., Mirsaeidi, M., Annesi-Maesano, I., . . . & Balmes, J. R. (2023). Impact of global climate change on pulmonary health: susceptible and vulnerable populations. Annals of the American Thoracic Society, 20(8), 1088-1095. https://doi.org/10.1513/AnnalsATS.202212-996CME
Blood A, B. A., Speicher M, Farmakidis A. (2024, November 8-12). State of the Curriculum: Findings from the AAMC and AACOM Curriculum SCOPE Survey [Conference Presentation]. Learn, Serve, Lead: AAMC Annual Meeting, Atlanta, GA, United States.
Fidler, L., Green, S., & Wintemute, K. (2022). Pressurized metered-dose inhalers and their impact on climate change. Canadian Medical Association Journal, 194(12), E460-E460. https://doi.org/10.1503/cmaj.211747
Frank, S. M., Jaacks, L. M., Meyer, K., Rose, D., Adair, L. S., Avery, C. L., & Taillie, L. S. (2024). Dietary quality and dietary greenhouse gas emissions in the USA: a comparison of the planetary health diet index, healthy eating index-2015, and dietary approaches to stop hypertension. International Journal of Behavioral Nutrition and Physical Activity, 21(1), 36. https://doi.org/10.1186/s12966-024-01581-y
Ghosh, A. K., Azan, A., Basu, G., Bernstein, J., Gillespie, E., Gordon, L. B., . . . & SGIM Environmental Health Interest Group, Medical Education Committee. (2024). Building climate change into medical education: A society of general internal medicine position statement. Journal of General Internal Medicine, 39(13), 2581-2589. https://doi.org/10.1007/s11606-024-08690-1
Gupta, J., Bai, X., Liverman, D. M., Rockström, J., Qin, D., Stewart-Koster, B., . . . & Gentile, G. (2024). A just world on a safe planet: a Lancet Planetary Health-Earth Commission report on Earth-system boundaries, translations, and transformations. The Lancet Planetary Health, 8(10), e813-e873. https://doi.org/10.1016/S2542-5196(24)00042-1
Haines, A. (2017). Health co-benefits of climate action. The Lancet Planetary Health, 1(1), e4-e5. https://doi.org/10.1016/s2542-5196(17)30003-7
Kazi, D. S., Katznelson, E., Liu, C. L., Al-Roub, N. M., Chaudhary, R. S., Young, D. E., . . . & Rice, M. B. (2024). Climate change and cardiovascular health: a systematic review. JAMA Cardiology, 9(8), 748-757. https://doi.org/10.1001/jamacardio.2024.1321
Laney, E., Rabin, B., & Philipsborn, R. (2022). Climate resources for health education implementation guide: A co-creation model for students and educators implementing and adapting CRHE resources. 15. https://climatehealthed.org/implementation-best-practices/
Lemery, J., O’Connor, T., Gillespie, E., Blackburn, H., Demorest, S., Philipsborn, R., & Chekuri, B. (2024). Opportunities for Strengthening Climate Education for Clinical Health Professionals. NAM Perspectives, 2024, 10-31478. https://doi.org/10.31478/202409b
Liu, I., Rabin, B., Manivannan, M., Laney, E., & Philipsborn, R. (2022). Evaluating strengths and opportunities for a co-created climate change curriculum: Medical student perspectives. Frontiers in Public Health, 10, 1021125. https://doi.org/10.3389/fpubh.2022.1021125
Or, Z., & Seppänen, A. V. (2024). The role of the health sector in tackling climate change: A narrative review. Health Policy, 143, 105053. https://doi.org/10.1016/j.healthpol.2024.105053
Rabin, B. M., Laney, E. B., & Philipsborn, R. P. (2020). The unique role of medical students in catalyzing climate change education. Journal of Medical Education and Curricular Development, 7, 2382120520957653. https://doi.org/10.1177/2382120520957653
Romanello, M., Walawender, M., Hsu, S. C., Moskeland, A., Palmeiro-Silva, Y., Scamman, D., . . . & Costello, A. (2024). The 2024 report of the Lancet Countdown on health and climate change: facing record-breaking threats from delayed action. Lancet, 404(10465), 1847-1896. https://doi.org/10.1016/s0140-6736(24)01822-1
Salas, R. N., & Solomon, C. G. (2019). The climate crisis – health and care delivery. New England Journal of Medicine, 381(8), e13. https://doi/10.1056/NEJMp1906035
Smirnova, N., Shaver, A. C., Mehta, A. J., Philipsborn, R., & Scovronick, N. (2023). Climate change, air quality, and pulmonary health disparities. Clinics in Chest Medicine, 44(3), 489-499. https://doi.org/10.1016/j.ccm.2023.03.005
Whitmee, S., Haines, A., Beyrer, C., Boltz, F., Capon, A. G., de Souza Dias, B. F., . . . & Yach, D. (2015). Safeguarding human health in the Anthropocene epoch: report of The Rockefeller Foundation-Lancet Commission on planetary health. The Lancet, 386(10007), 1973-2028. https://doi.org/10.1016/S0140-6736(15)60901-1
Willett, W., Rockström, J., Loken, B., Springmann, M., Lang, T., Vermeulen, S., & Murray, C. J. L. (2019). Food in the Anthropocene: The EAT-Lancet Commission on healthy diets from sustainable food systems. The Lancet, 393(10170), 447-492. https://doi.org/10.1016/s0140-6736(18)31788-4
Assistant Professor, Department of Family & Preventive Medicine, Emory University School of Medicine, ryan.d.smith@emory.edu
ORCID-ID 0000-0001-9143-8937
Medical Student, Emory University School of Medicine
Associate Professor, Department of Medicine, Emory University School of Medicine
ORCID-ID 0009-0005-7672-4843
Published: 7/21/25